|
 |
 |
When a problem such as fibroids requires the removal of your uterus, having it done with a scope through buttonhole size incisions makes for a less painful, rapid recovery. Your ovaries are usually preserved, maintaining normal hormone and sexual function.
If you’re like most women, the thought of a hysterectomy means a long recovery and a large visible scar. It used to be that Total Abdominal Hysterectomy (removal of the uterus and cervix through a large abdominal incision) was the only type of hysterectomy offered to women. But today innovative laparoscopic techniques and the development of improved surgical devices allow for less invasive procedures. Consequently, hospital stays, and recovery times, have also been significantly reduced.
Honestly few OBGyns are trained to perform Laparoscopic Hysterectomy or do so frequently enough to hone their skills in this technically advanced procedure. In fact Dr. Scott Kramer was among the first to perform Laparoscopic Hysterectomy in the Bay Area (1993) and continues as one of the most experienced surgeons having performed hundreds of them.
Let’s compare different types of hysterectomy: Total Abdominal Hysterectomy (TAH) is an “open” procedure performed through a large 6 to 8 inch incision to remove the uterus. Laparoscopic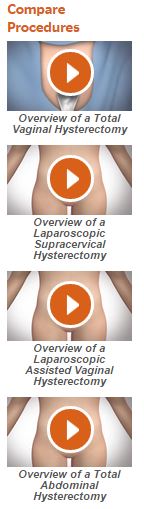 Hysterectomy has variations. The uterus can be completely removed during a Total Laparoscopic Hysterectomy (TLH) or Laparoscopic Assisted Vaginal Hysterectomy (LAVH), which are essentially the same operation. Or where the cervix (the part of the uterus that attaches to the vagina) is preserved, called Laparoscopic Supracervical Hysterectomy (LSH). Finally, Total Vaginal Hysterectomy (TVH) is considered the original minimally invasive hysterectomy. It is similar to TLH but without any abdominal incisions. With all these procedures we can leave your ovaries in place, preserving female hormones, and only remove the diseased uterus. The option to remove the fallopian tubes, which reduces the subsequent risk for developing ovarian cancer, can usually be accommodated with all types of hysterectomy.
Hysterectomy has variations. The uterus can be completely removed during a Total Laparoscopic Hysterectomy (TLH) or Laparoscopic Assisted Vaginal Hysterectomy (LAVH), which are essentially the same operation. Or where the cervix (the part of the uterus that attaches to the vagina) is preserved, called Laparoscopic Supracervical Hysterectomy (LSH). Finally, Total Vaginal Hysterectomy (TVH) is considered the original minimally invasive hysterectomy. It is similar to TLH but without any abdominal incisions. With all these procedures we can leave your ovaries in place, preserving female hormones, and only remove the diseased uterus. The option to remove the fallopian tubes, which reduces the subsequent risk for developing ovarian cancer, can usually be accommodated with all types of hysterectomy.
Both TLH/LAVH and VH involve the removal of the entire uterus, including the cervix, through the vagina (like delivering a baby). Then the incision at the top of the vagina is closed with dissolvable stitches. So it’s important to abstain from intercourse or straining activities for 6 weeks as this incision heals.
LSH affords better pelvic support, because the ligaments that support the cervix and vagina are left intact. LSH also causes less vaginal dryness because the glands of the cervix continue to secrete mucous. However PAP smear screening for cervical cancer needs to continue after LSH, but the odds of developing this decline as you age.
Currently there is controversy about utilizing powered morcellators during LSH to cut up the uterus inside the abdomen so it can be removed through small holes because of concerns about theoretically increasing the spread of an undiagnosed rare Uterine Cancer called Leiomyosarcoma. The best estimates are this rare cancer occurs in 1 in 1550 fibroid uteri removed during hysterectomy. The FDA inaccurately estimated a lower figure (ACOG letter to FDA: Morcellation Fibroid Uterus). Since the odds are very low it should in no way deter you from having a hysterectomy as a solution to a medical problem your uterus is causing. We have adopted an alternative technique to safely remove the fibroid uterus at the conclusion of the hysterectomy, placing it in a tough plastic bag, then cutting it into long strips outside the body.
Most importantly, both types of Laparoscopic Hysterectomy result in significantly less pain and a quicker recovery compared to traditional hysterectomies because of the small incisions used in the laparoscopic approach. Consequently they are usually performed at the outpatient surgery center, which has private suites. Sparing of the ovaries in most cases, avoids the need for hormone replacement.
The Numbers Tell The Story …
| Type of Hysterectomy | Incision Site | Average Hospital Stay | Average Recovery Time |
| Abdominal Hysterectomy (TAH) |
6-8 inch abdominal incision |
3-4 days | 6 weeks (42 days) |
| Vaginal Hysterectomy (TVH) |
No abdominal incision (only vaginal) |
1 day or less | 7-14 days |
| Laparoscopic Hysterectomy (LSH, TLH, & LAVH) |
3-4 tiny (1/4 inch) abdominal incisions |
1 day or less | 7-14 days |
Robotic Hysterectomy = Laparoscopic Hysterectomy
Sounds cool, but… Despite the compelling marketing hype by many hospitals and physicians are trying to recoup their multi‑million dollar investment.robotic hysterectomy, is simply using a “tool” to perform a laparoscopic hysterectomy. The benefits are identical: less postoperative pain, tissue trauma, blood loss, scarring; and a faster return to normal activities, compared to more traditional open hysterectomy. The robot enables those surgeons unable to perform a laparoscopic hysterectomy to convert an open procedure to a minimally invasive surgery. However, it takes an additional 45 minutes under anesthesia to set up the robot and costs the patient thousands of dollars. In 2013, the American College of Obstetricians & Gynecologists published an official statement that there are really are no additional benefits (except for cancer surgery).
Click here to learn more about Robotic Hysterectomy
Honestly, many OBGyns are so busy delivering babies that they realistically don’t have time to more than dabble in minimally invasive surgery. So why not seek a gynecologist who is an experienced, skilled laparoscopic surgeon?
While hysterectomy should be our last resort to resolve a gynecologic problem, if you do need one then ask “Why not a Laparoscopic Hysterectomy?”