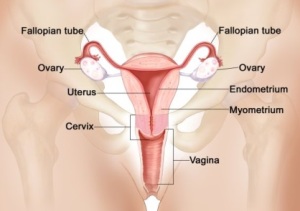
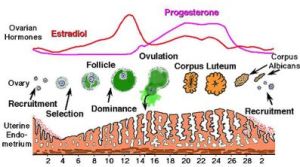
The uterus has two layers. The thick outer muscular layer and the thin inner layer called the endometrium. The ovary produces female hormones that stimulate the endometrium to grow thick each month in preparation for pregnancy. If a woman does not become pregnant, the lining sheds during the menstrual period. After menopause, without female hormones, the lining stops growing and shedding.
How do you know when bleeding during your period is abnormally heavy? The easiest way to determine this is note how often you need to change your pad or tampon. If you have to change less than every two hours, or if you have a period that lasts more than 7 days your periods are abnormally heavy. Other clues that signify you have excessive menstrual flow:
- Blood leaking through to stain clothes or bedding
- You need double sanitary protection (tampons and pads)
- Frequent bleeding between periods
- You pass large blood clots
- Your period disrupts your daily activities (e.g. Inability to exercise, workplace distraction)
Since the World Health Organization estimates that 1 in 5 women will suffer with heavy periods at some point during her reproductive years we will take time to cover this in detail. Over the next month I will send you a weekly newsletter describing each of the common causes of heavy periods and specific treatment options. Stay tuned…
If you’re curious here’s a preview of one of the most popular and effective treatments that can be performed in our office in 90 seconds to eliminate heavy periods!
Let’s take look at the most common causes of heavy menstrual bleeding:
A hormonal imbalance is the most common cause of heavy menstrual bleeding, especially during adolescence or approaching menopause. This also goes by the term Polycystic Ovarian Syndrome (PCOS), which is not a problem with cysts; but rather the absence of ovulation and therefore cyclic progesterone hormone production. While the unpredictable bleeding history alone is usually sufficient to make a diagnosis, blood tests can help exclude other hormonal causes such as thyroid dysfunction.
Solutions:
- If pregnancy is immediately desired then “fertility drugs” can usually induce ovulation. This has become a specialty on its own and should be administered and monitored by a Reproductive Endocrinologist who has many options to treat infertility.
- Replacing missing progesterone, either cyclically or more commonly using birth control pills, will usually reestablish a predictable period with modest flow. Alternatively the Mirena® IUD delivers progesterone directly to the endometrium to reduce menstrual bleeding.
Uterine fibroid tumors are another very common cause of excessive menstruation. It’s important to understand that fibroid tumors are almost always benign (non-cancerous) muscle tumors that occur in the uterus of women during their 30’s and 40’s. While the cause of fibroids is unclear, it is clear that they are estrogen-dependent, so will shrink after menopause. Fibroids can be readily detected during a pelvic sonogram. No intervention is necessary for fibroids that don’t cause symptoms.
Solutions: Several surgical treatments are available for treating fibroids that cause symptoms of heavy bleeding, pressure, pain, discomfort with sex, and urinary frequency:
- While there is currently no medication that eradicates fibroids, hormonal therapy such as birth control pills or the progesterone IUD called Mirena® may reduce menstrual flow making periods tolerable and avoiding surgery.
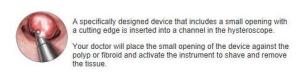
- Myomectomy is an operation where only the fibroids are removed, preserving the uterus for childbearing. If the fibroid is confined inside the uterine cavity then this can be accomplished without any incisions by inserting a hysteroscope through the cervical opening and then shaving the tumor away.
- Uterine artery embolization involves threading a thin tube into the blood vessels that supply the uterus and injecting foam to temporarily block the blood flow. The fibroids then shrink. Pregnancy is not recommended afterwards.
- Hysterectomy: With the conservative treatments listed above there is about a 1 in 4 chance of fibroid recurrence that will require surgery in the future. Hysterectomy is removal of the uterus containing the fibroid tumors, preserving the ovaries and hormonal function. It is usually recommended for women who have completed their families. Honestly, the only consequences are no more babies and no more periods. Many women report improved sex afterwards. Increasingly minimally invasive hysterectomy can be performed by a skilled gynecologist, allowing a rapid, less painful, recovery.
Polyps are small, fragile growths from the inner lining of a body cavity.
Cervical polyps protrude from the cervical canal into the upper vagina, where they can be seen during a pelvic exam. Many women do not have symptoms and the polyp is found during a routine annual pelvic exam. Others report symptoms of bleeding, typically after sex or between periods. With very rare exception cervical polyps are benign.
Solutions:
- Cervical polyps can be painlessly removed in seconds during an office visit.
Endometrial polyps protrude from the inner lining of the uterus. The cause of endometrial polyps is unclear, although they are often associated with excess or unopposed (no progesterone) estrogen. In most women they are typically non-cancerous growths, but the chance for malignancy increases with the size of the polyp, and especially after menopause.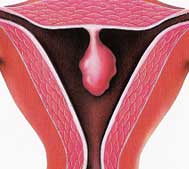
In a in a modern equipped gynecologist’s office like ours we have two methods to detect endometrial polyps:
1) Enhanced pelvic ultrasound, called a Saline Infused Sonogram
2) A hysteroscope; a thin scope that is inserted into the uterine cavity to visualize growths
Solutions:
Using the hysteroscope endometrial polyps can be quickly removed during a 15 minute outpatient procedure. All tissue removed is sent to pathology for analysis. Patients return to normal activities the following day.
Endometrial (uterine) cancer is what most women fear when they experience abnormal uterine bleeding. It occurs when abnormal cells in the inner lining of the uterus, the endometrium, multiply out of control and invade the walls of the uterus, then later spread to other organs. While the cause of endometrial cancer is unknown, it is known that women diagnosed with this type of cancer are usually over fifty, frequently produce (eg. Obesity) or take unopposed estrogen (no progesterone). Uterine cancer typically presents as abnormal uterine bleeding: prolonged menstrual bleeding or more commonly bleeding after menopause. A quick office evaluation includes a pelvic sonogram and an endometrial (uterine) biopsy that can be accomplished during a single office visit.
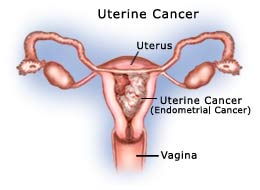
So don’t ignore abnormal uterine bleeding as it may be a warning sign that allows diagnosis at an early stage with a favorable prognosis for cancer‑free survival. Treatment for endometrial cancer is usually hysterectomy with removal of the fallopian tubes and ovaries; possibly followed by chemotherapy and/or radiation treatments only in more advanced cases.
In some scenarios other causes of abnormal uterine bleeding, such as a bleeding disorder due to abnormal coagulation need to be considered. Nevertheless many times after a thorough evaluation no cause for bothersome heavy periods can be detected. The good news is there are many options besides hysterectomy that should be tried first. This includes hormones such as birth control pills or progesterone, the Mirena® IUD, a non‑hormonal medication called Lysteda®, or an endometrial ablation.
Endometrial ablation is an ideal choice for women who have completed childbearing and don’t want to use hormones. The Novasure method involves a 90 second outpatient treatment where the inner uterine walls are cauterized so the endometrial lining does not grow back afterwards. Studies show that over 90% of women are satisfied with either a significant reduction or complete cessation of menstrual bleeding. It doesn’t affect a woman’s hormones. Most women return to regular activities the following day. Increasingly women choose to have their endometrial ablation in our office using local anesthesia and oral sedation. Other women prefer a light general anesthetic so we also perform it at an outpatient surgery center. Best of all endometrial ablation is covered by health insurance.
Don’t let heavy periods continue to interfere with quality of your life. Schedule an office visit where we can evaluate and then make customized treatment recommendations for you.
Wishing you good health,
Scott Kramer MD, FACOG, FACS










Speak Your Mind