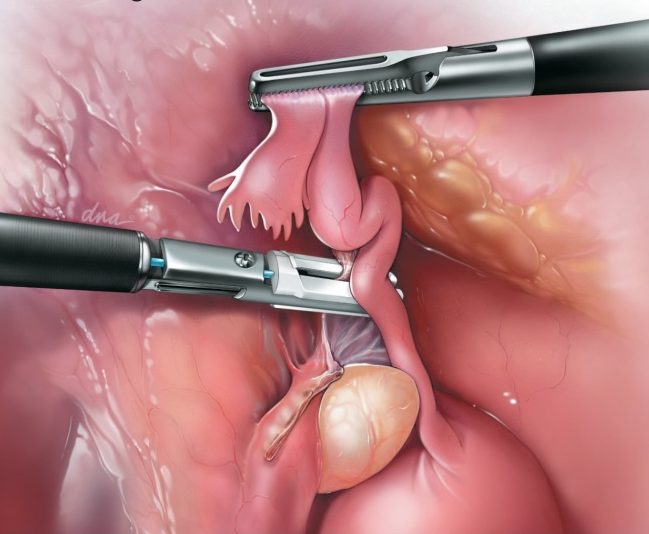
Recent recognition that many ovarian cancers actually arise from the fallopian tube requires a reassessment of our thinking about the management of the fallopian tubes at the time of surgery—Hysterectomy & Sterilization. The tubes serve no physiological role and provide no benefit to women in whom they are retained (unlike the ovary, where preservation may reduce mortality). The residual tube remains a possible site of infection, is at risk for torsion (twisting), is the most likely site for tubal pregnancy after sterilization failure; and also eliminates the conduit responsible for the backward passage of endometrial tissue (from inside uterine lining) into the pelvis during menstruation, reducing the risk of endometriosis. However, the most compelling benefit is that removing the fallopian tubes at the same time when other pelvic surgery is indicated becomes an opportunity to remove the source of some ovarian cancers.

Recent data from a Danish study of more than 13,000 ovarian cancer cases confirms that removing fallopian tubes reduces the risk of ovarian cancer by 42%. Removal of the tubes at the time of hysterectomy or tubal sterilization adds minimal risk to a planned surgical procedure, does not affect ovarian hormone production, and has the potential to greatly reduce the occurrence of our most deadly gynecologic malignancy. In addition, another landmark study revealed an unexpectedly high long-term failure rate after tubal sterilization (tubal ligation) of nearly 2%, many were potentially deadly tubal pregnancies. Removing the fallopian tubes is far more effective sterilization.
The time has come to require that all women who are undergoing gynecologic surgery after having completed childbearing should be counseled about the lack of benefit and possible harm from retaining their fallopian tubes. Removing the fallopian tubes should be recommended to all women undergoing hysterectomy (removal of the uterus) and it should be offered preferentially to women desiring permanent female sterilization in place of less effective alternatives (tubal ligation). All of these procedures can usually be accomplished via minimally invasive, outpatient surgery. Data supports the relative safety of these measures, and in the absence of effective screening, these simple changes in surgical practice can have a significant impact in the prevention of ovarian cancer.
While this is indeed a paradigm shift, OBGyns and patients should ask themselves, “Why keep an organ with no ongoing physiological role when it can be safely removed at the time of planned surgery and leaving it in place puts a woman at risk for a potentially preventable cancer?”
Wishing you good health!
Scott Kramer MD, FACOG







Speak Your Mind